Guest post: The ultimate explanation for why the CMI is so low

MD, CCS, CCDS
By Kamran H. Shah, MD, CCS, CCDS
The question most frequently asked of CDI programs, in my experience, is why the case mix index (CMI) is so low. The asker is different from facility to facility—the question may come from the C-suite (chief executive officer, financial officer, medical officer, vice president of revenue cycle, etc.)—but the question always remains the same.
Sometimes, CDI programs are optimistic about their performance in a particular month—their monthly report shows high CDI productivity, an excellent shift in CMI from working to final coded MS-DRG, and a positive reimbursement trends resulting from queries. On the other side, the revenue cycle team may have concerns about a low overall hospital CMI for the same month and looking for justification.
In this scenario, revenue cycle is looking at data and CMI from a different perspective and, in their minds, the ultimate responsibility for the facility’s CMI falls on the shoulders of the CDI program. If the hospital’s CMI is low in a particular month, all eyes are focused on CDI for an explanation.
Traditionally, the CDI program would combat these questions about low CMI by providing their positive metrics in other areas (e.g., the number of charts reviewed, the number of queries that affected the final DRG assignment, the number of queries that affected the severity of illness or risk or mortality, CDI/coder DRG matches, etc.). These reports, however, rarely satisfy hospital administration.
Imagine that you have a consistent CDI team that’s performing well and there’s no significant change in the service lines. When you’re asked why the CMI has suddenly taken a down turn, one option is to do a relative weight (RW) distribution analysis, such as shown in the following graph.
RW distribution (initial/working CMI) monthly comparison report
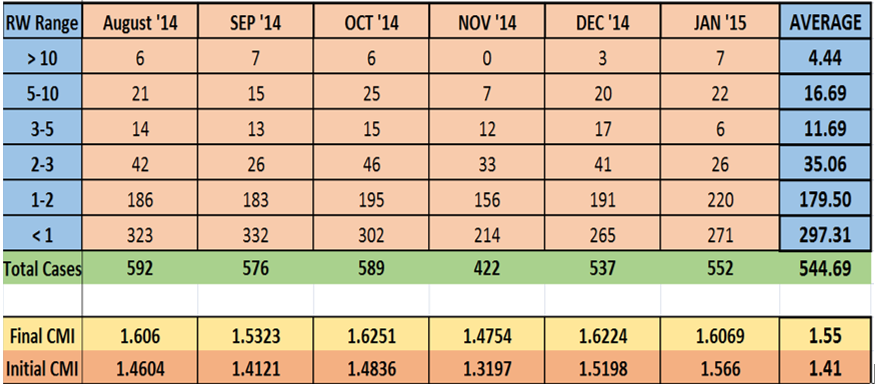
Through this analysis, you can compare weekly/monthly discharge cases by dividing them by different RW categories. The distribution of cases will help you understand why the initial CMI (i.e., working CMI) was low in a particular month.
Personally, I’ve seen great responses and appreciation to this report. I highly recommend making this part of your regular CDI reports, especially if the administration is concerned about the efficacy of the CDI program when it comes to the facility’s CMI. You can enhance this report further by creating RW distributions for final CMI for the same cases and show how the CDI team was able to move cases to a higher RW.
Editor’s note: Dr. Shah is the senior consultant at ARK HIM SOLUTIONS. Contact him at kshah@ARK360.co. Opinions expressed are that of the author and do not necessarily represent HCPro, ACDIS, or any of its subsidiaries.
